Friday, Jan 27
This is one of a five part series of a visit to Mekelle, Tigray and Addis Ababa in January 2024. Below are links to the series, or you can just follow the “next” and “previous” links at the bottom. You can send a message to the author here.
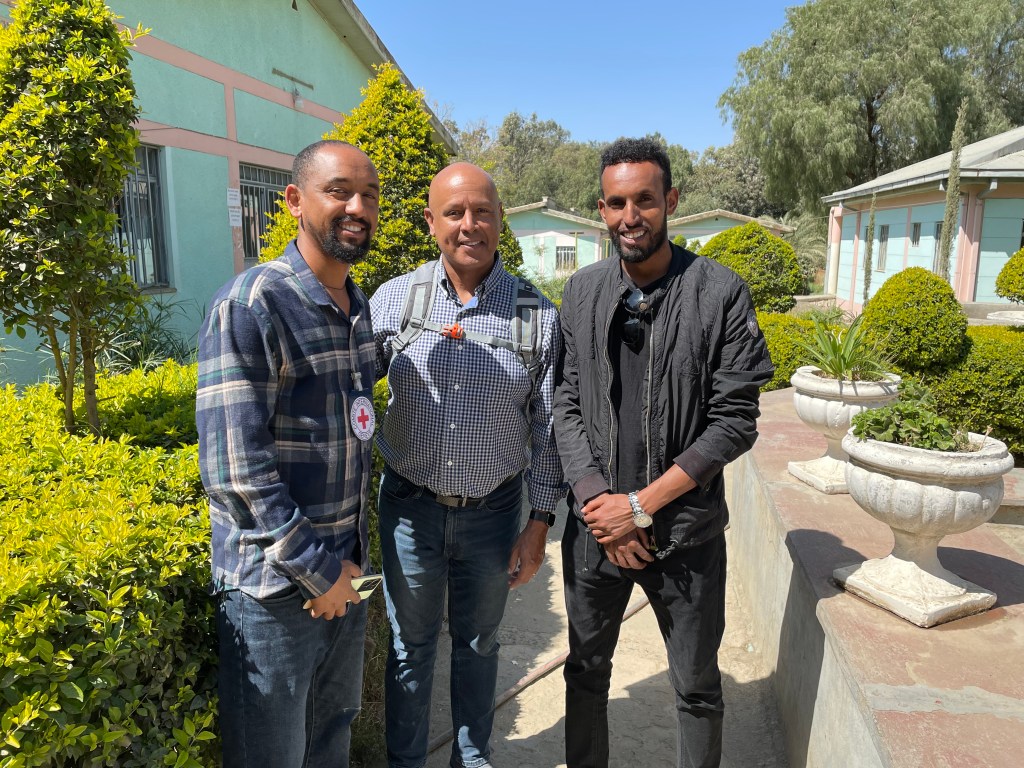
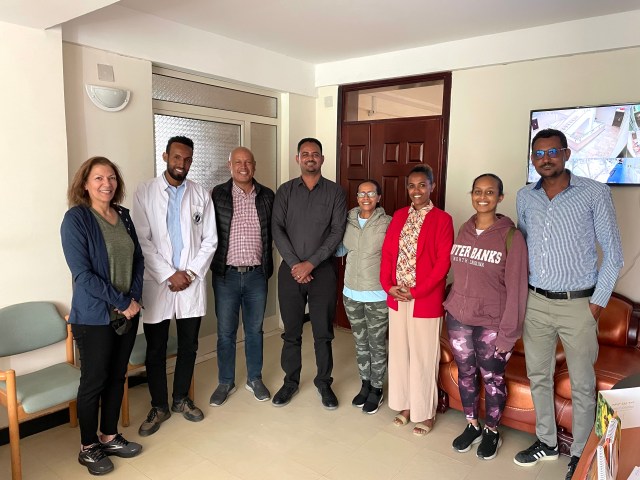
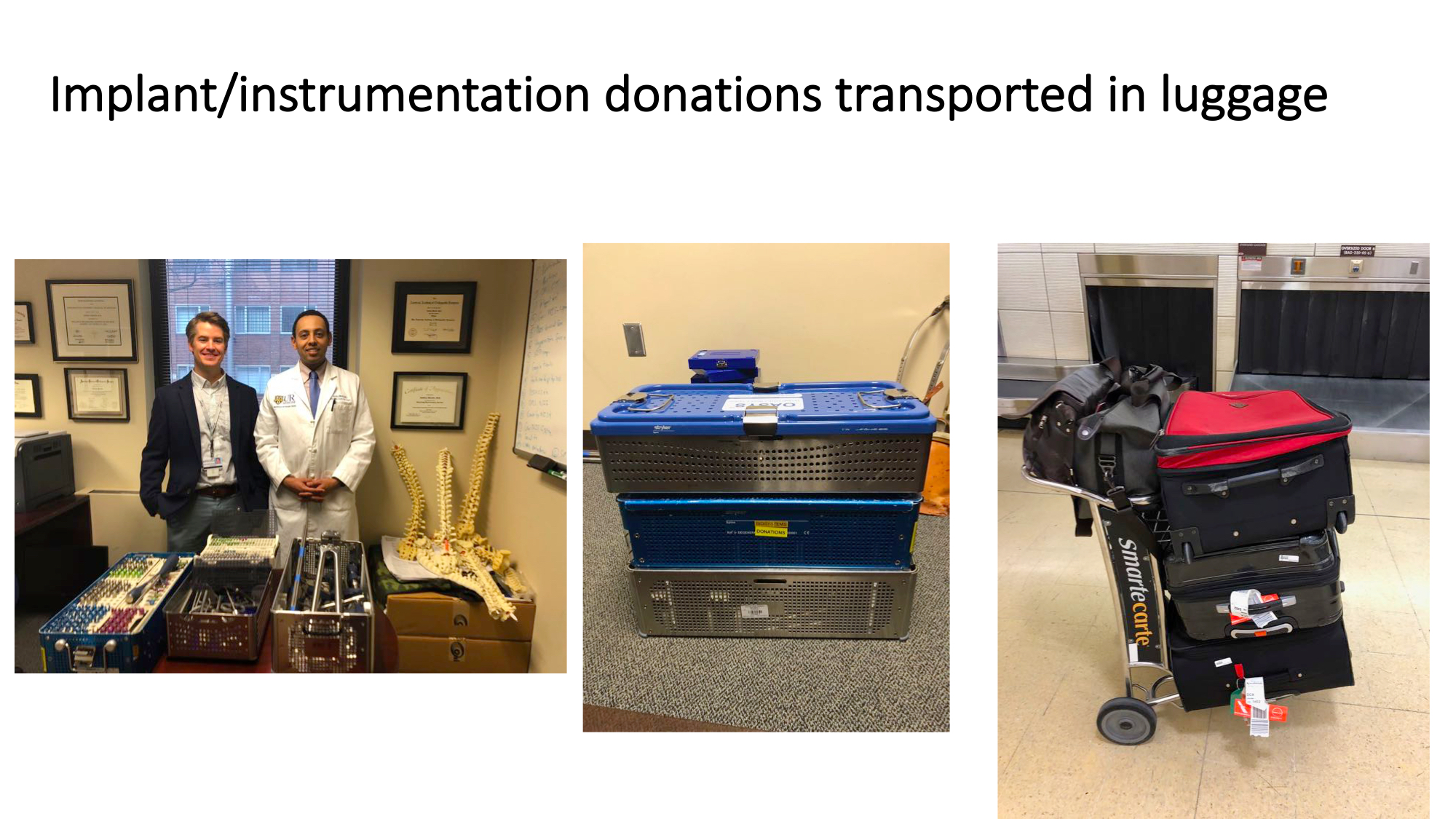
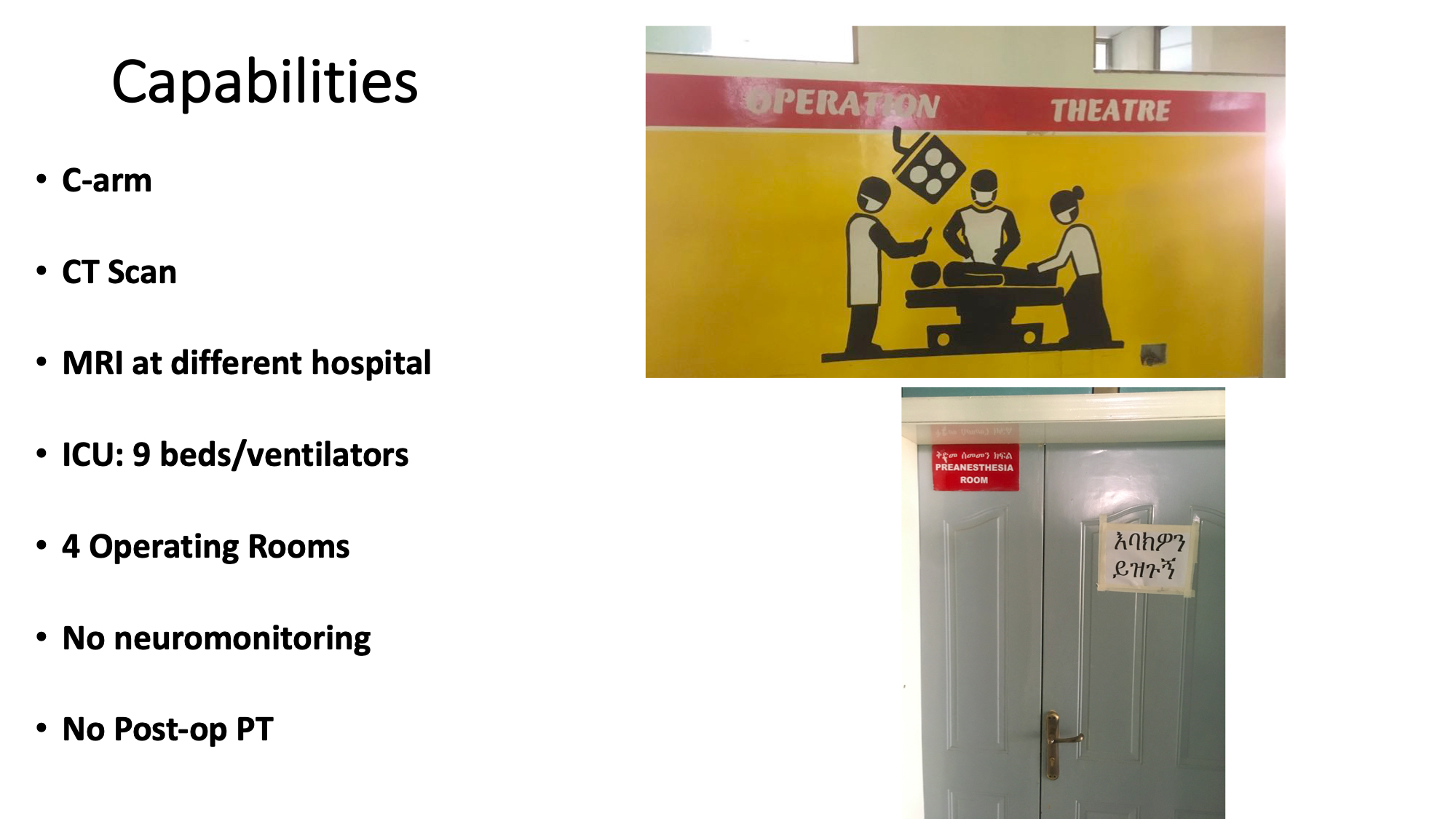
On returning to Addis, I went directly to AaBET hospital, which I had visited in 2019 with a small team of docs. Dr Mamo was my host then, and it was great to see him again and catch up. Five years ago, when I arrived, there was no sports orthopedist in the country. At that time, Dr Mamo was about to complete his sports fellowship in Egypt. Dr. Wiemi Douoguih from Washignton DC was part of our team and very generously donated an arthroscopy tower and some knee ligament reconstruction implants. A couple of years later, I sent another supply of implants when they ran out. The hospital was able to provide them new cameras when they were needed.
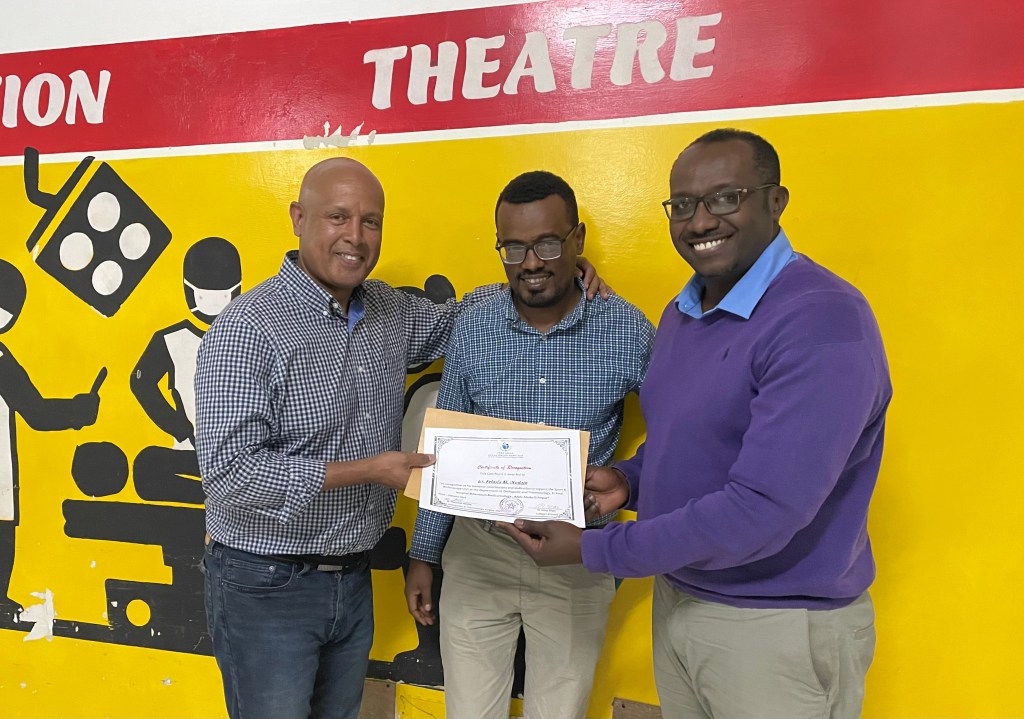
Dr Mamo started a sports orthopedics program from scratch on his return, using the arthroscopy equipment and implants. Shortly after, he was joined by another sports fellowship grad. Initially they had no patients, but little by little their practice started to pick up. In a few years, they had more patients than they could handle and now have a 1000 patient waiting list. While I was visiting, Dr Mamo learned that the Ethiopian Sports Federation wants to partner with them to send their athletes directly to them. It was amazing to hear how a little help led to such a big effect. The CEO of the hospital came by to join us and then presented to me a certificate of thanks, which was unexpected. Currently, because they’ve run out of implants and have a broken shaver head, so they are not doing arthroscopies. I am going to try to get them replacements.

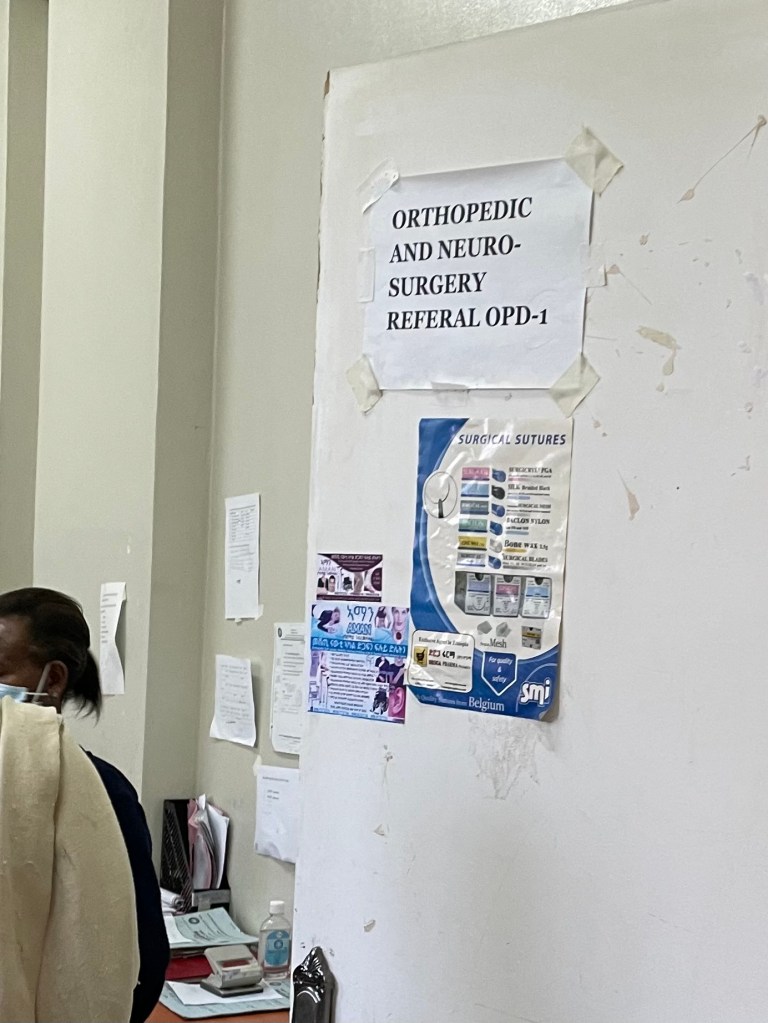
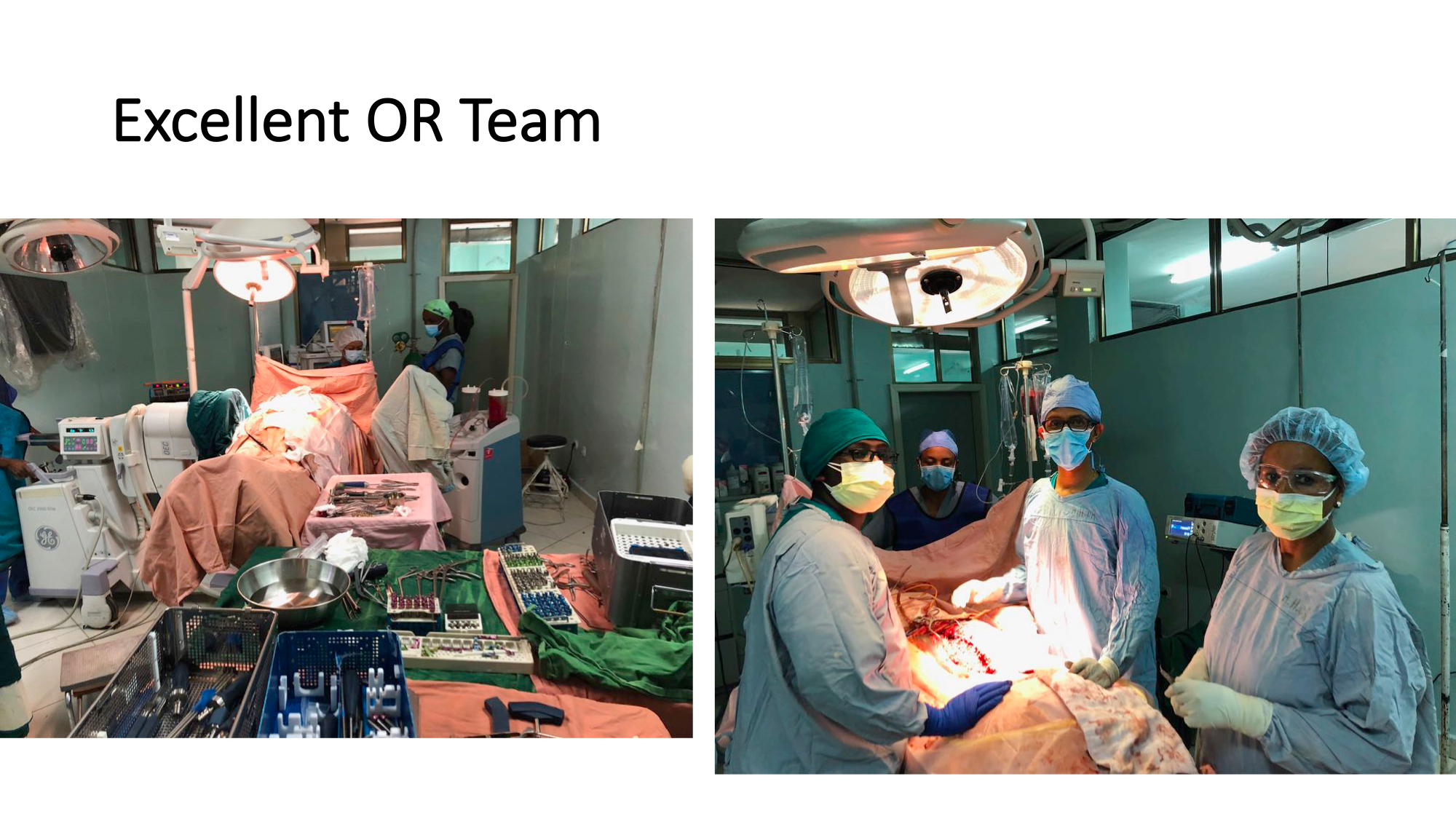
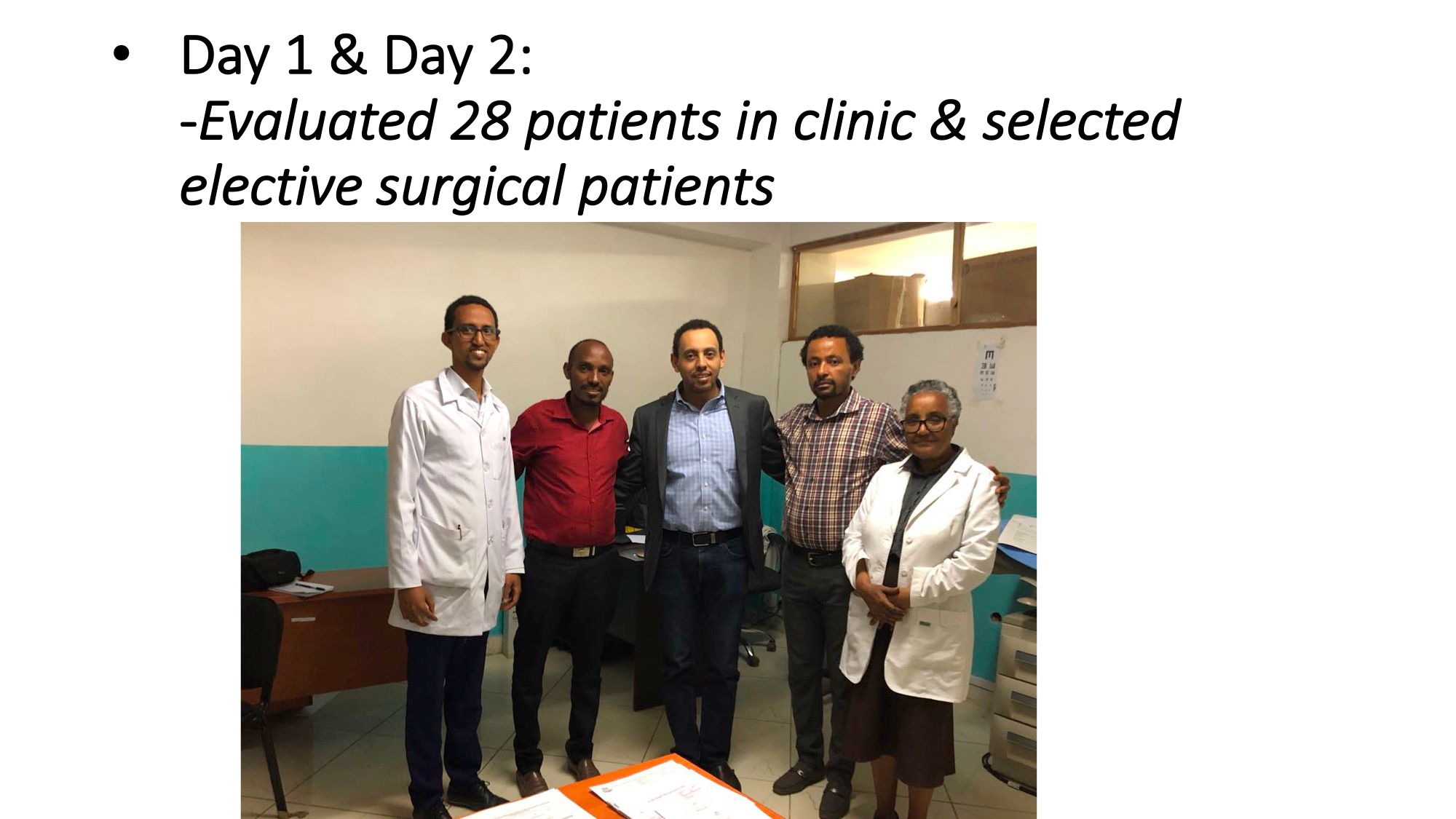
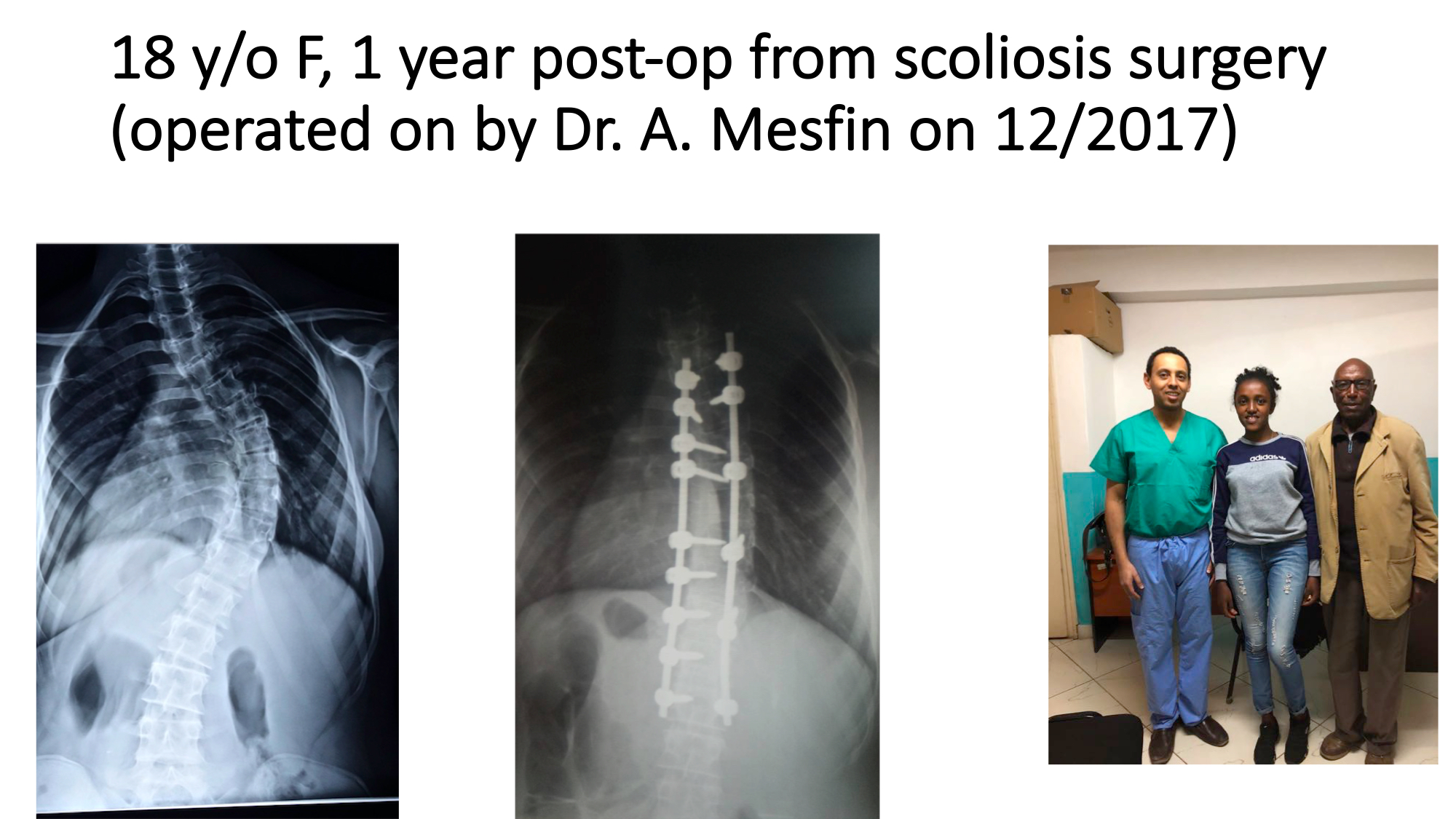
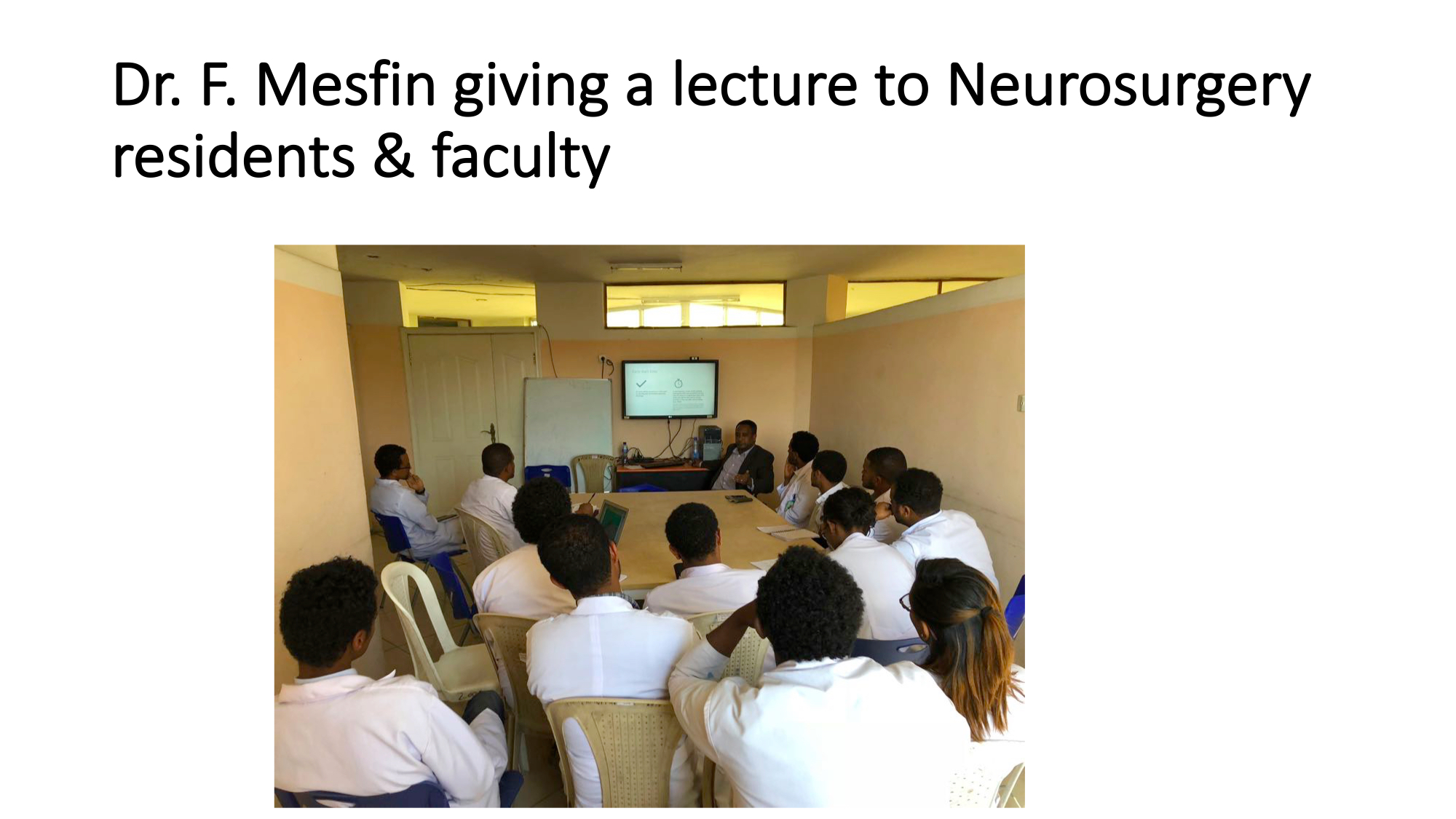
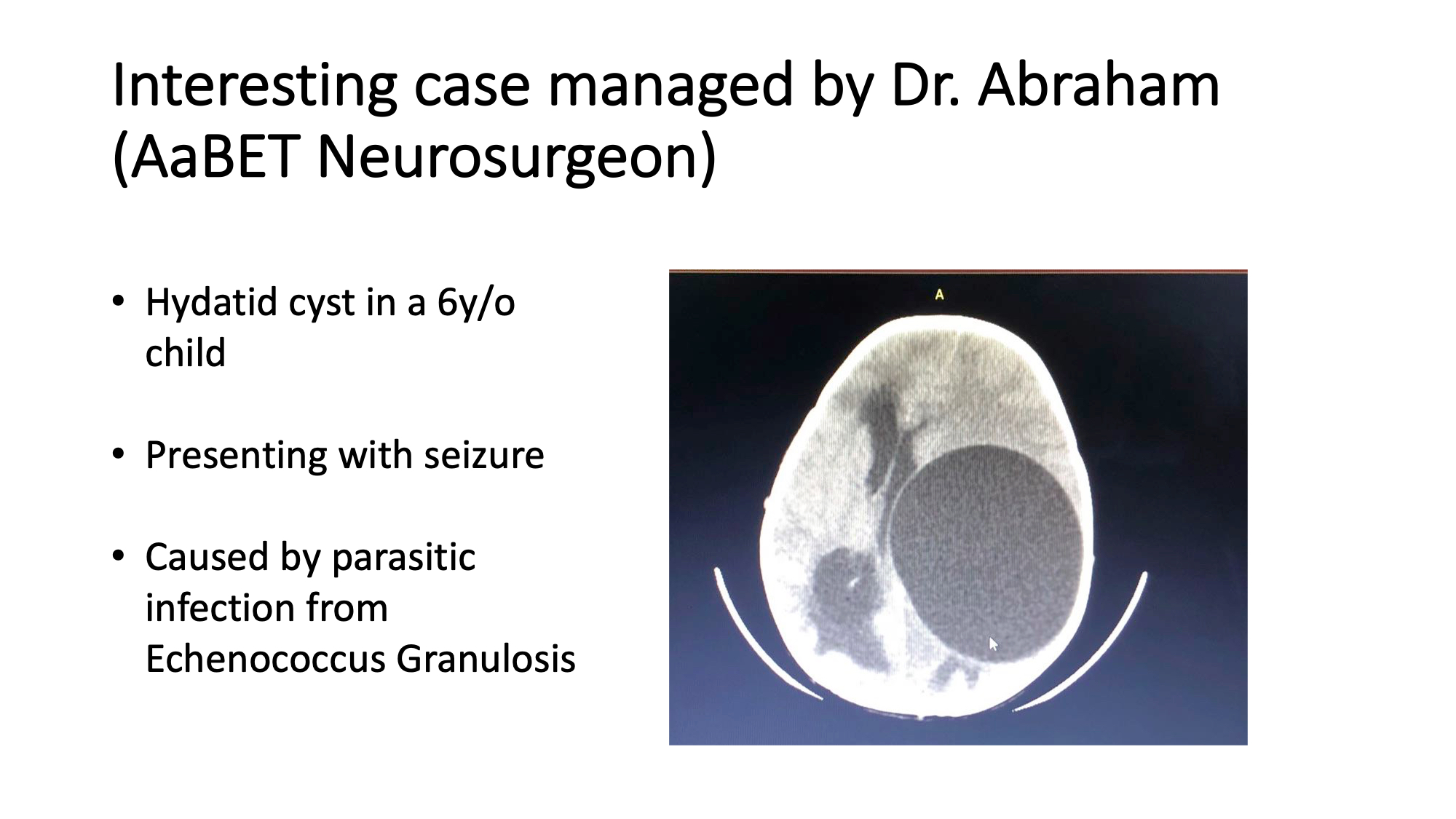
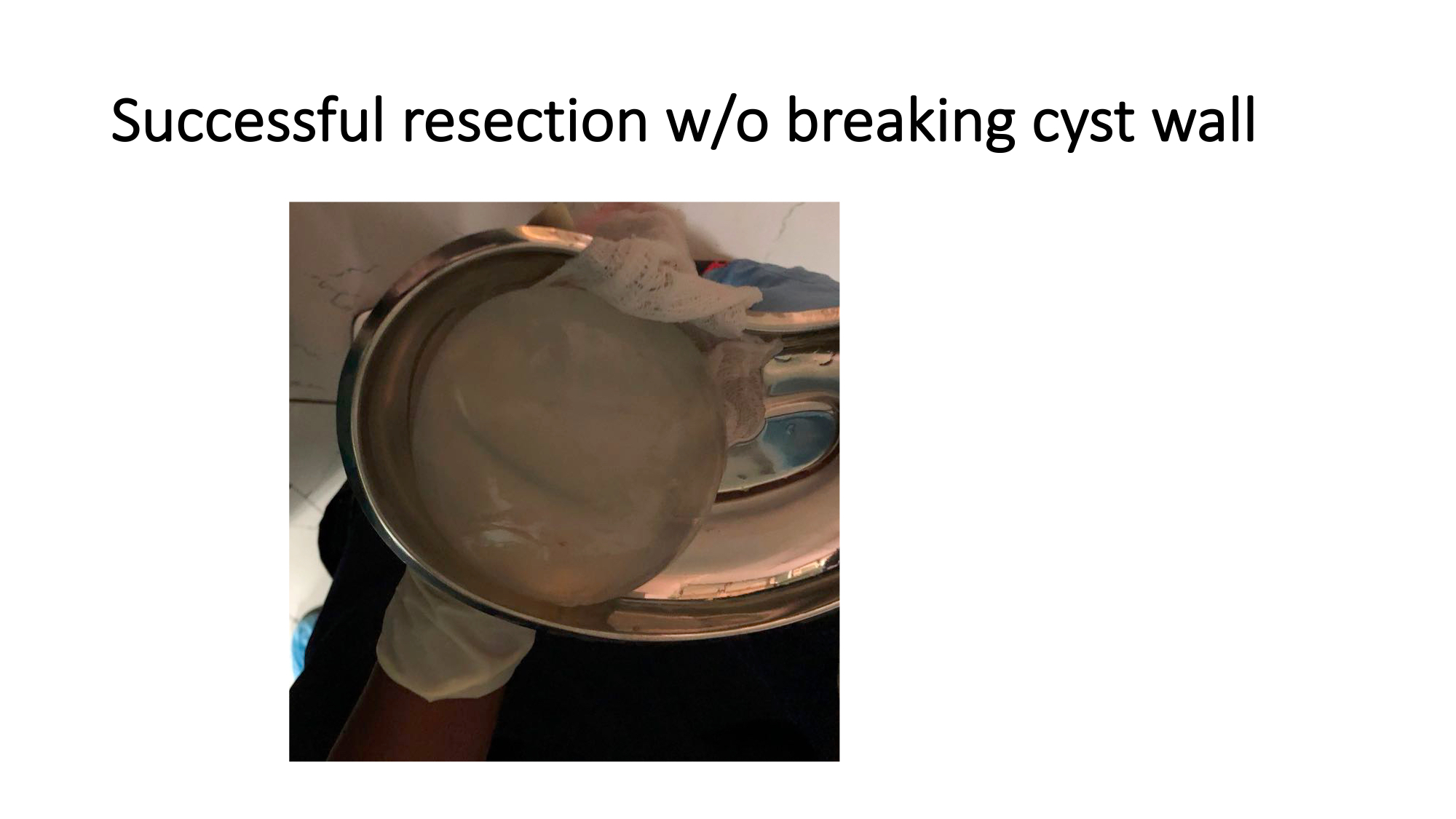
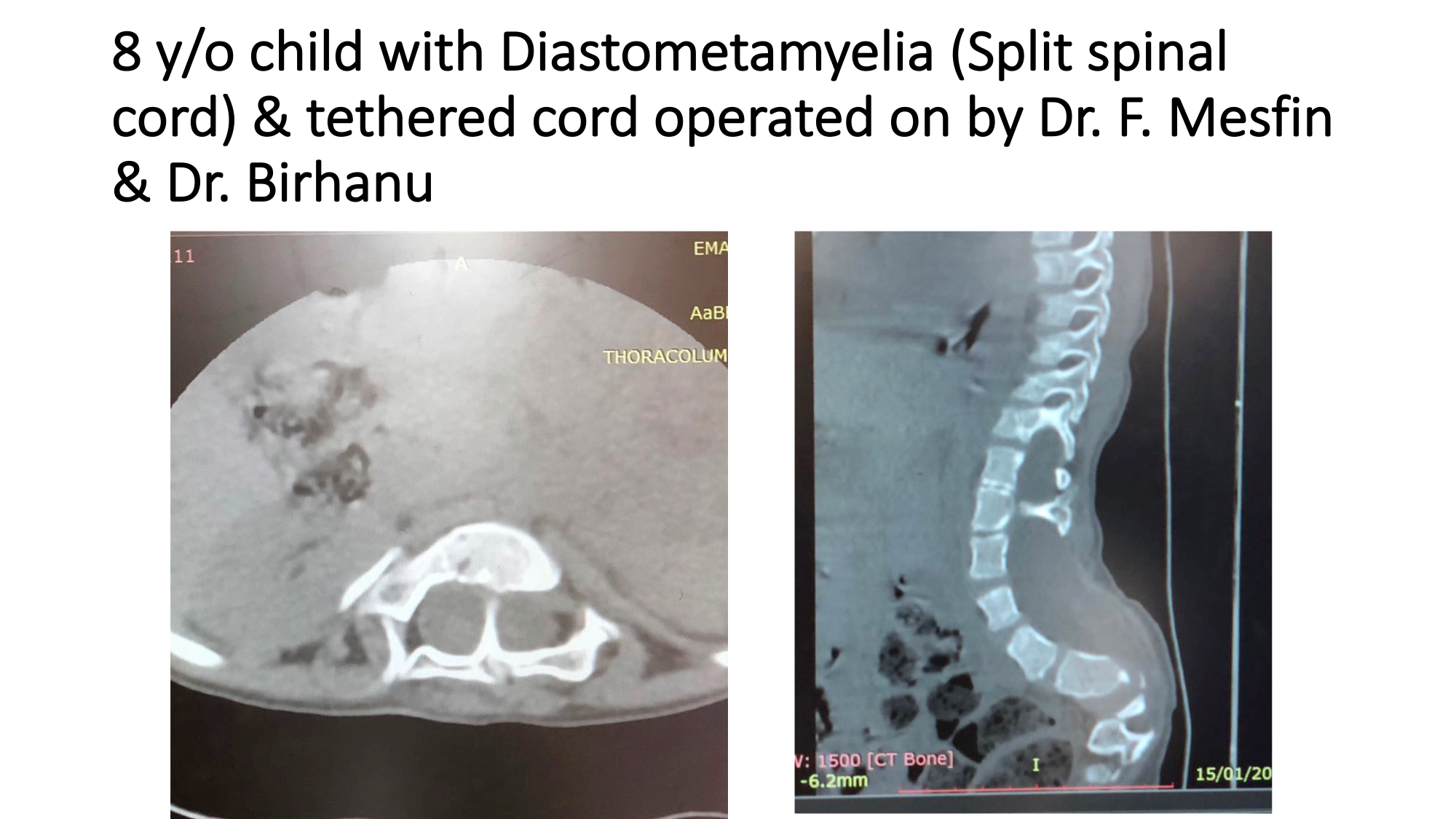
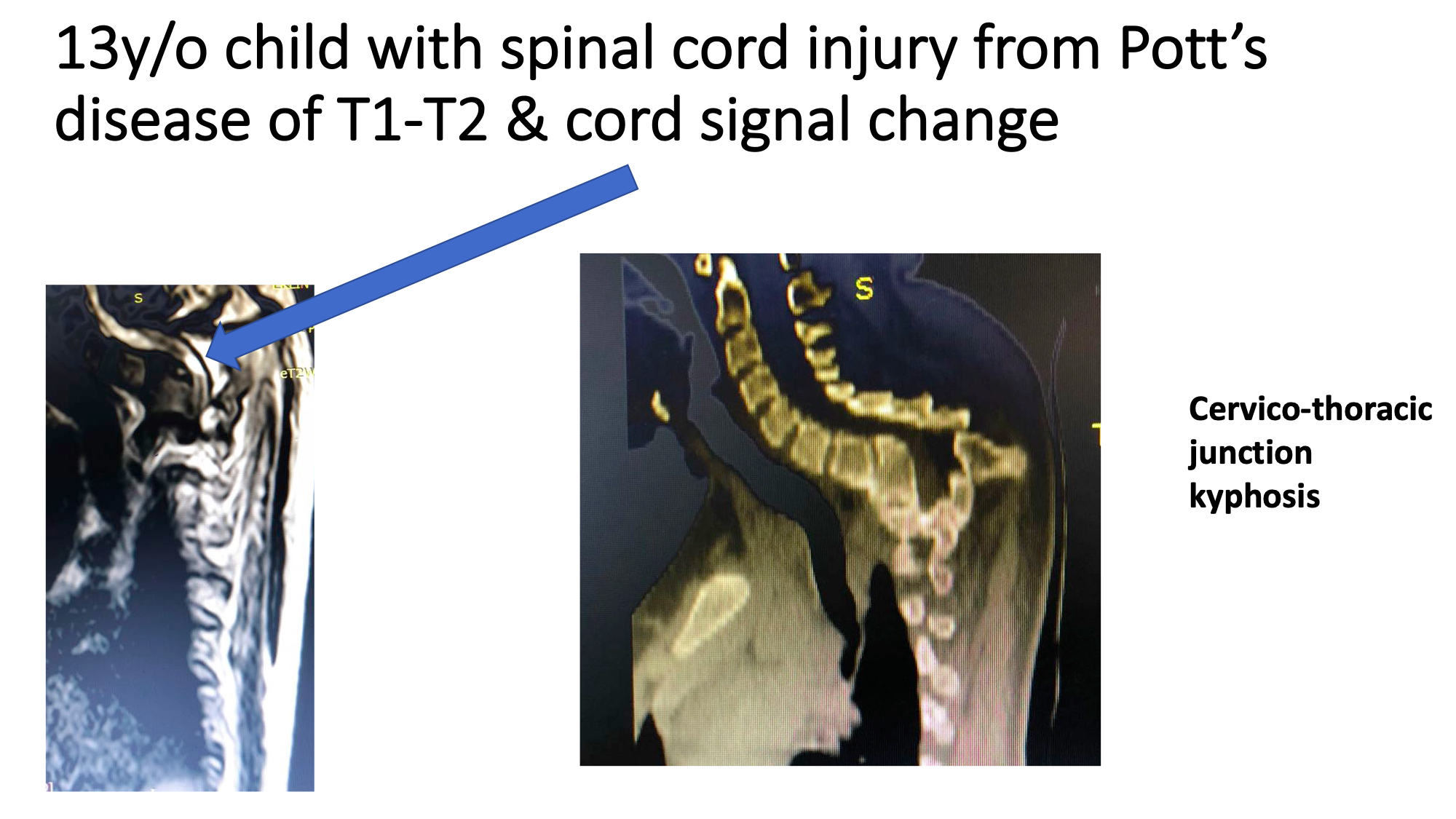
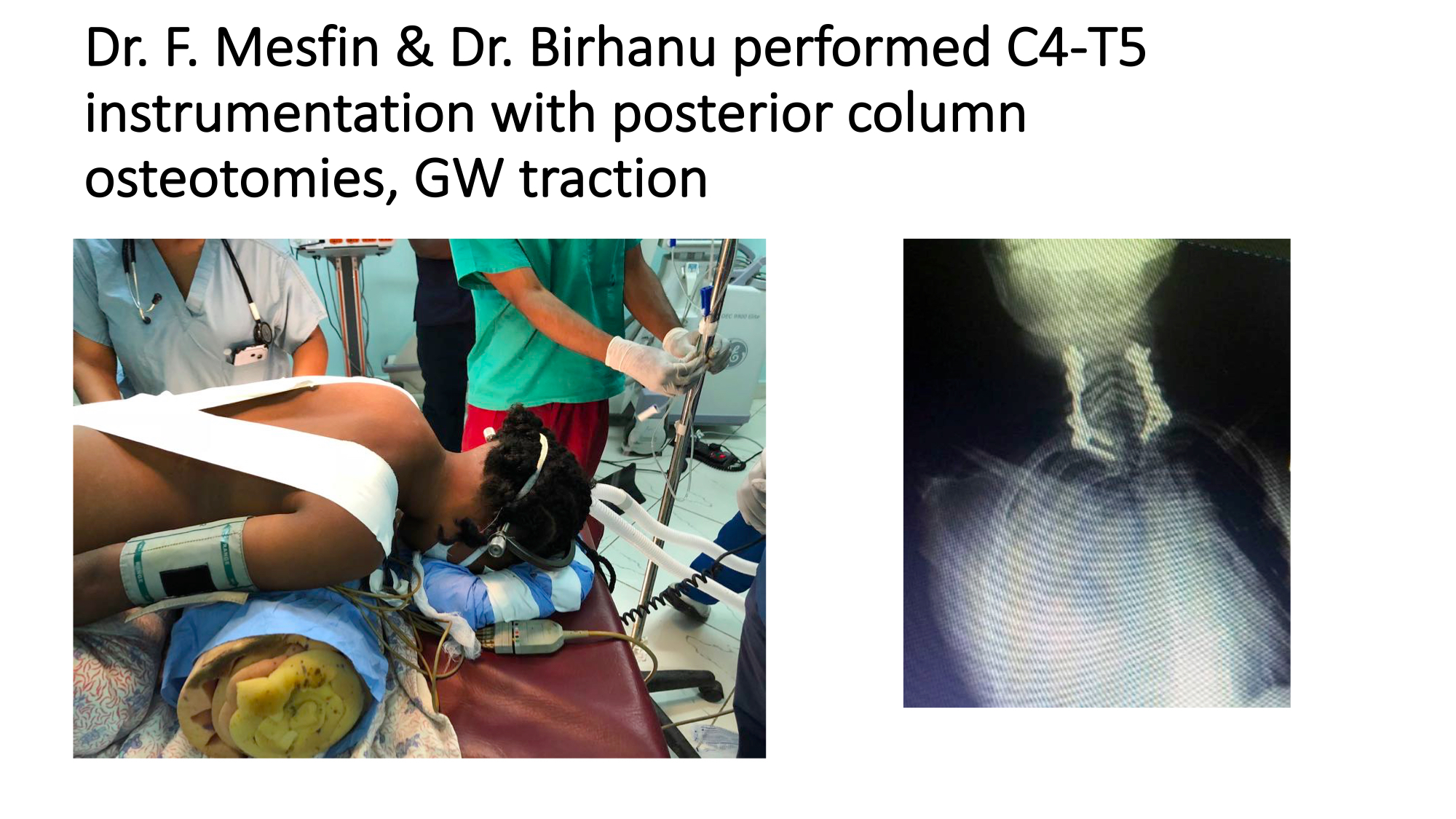
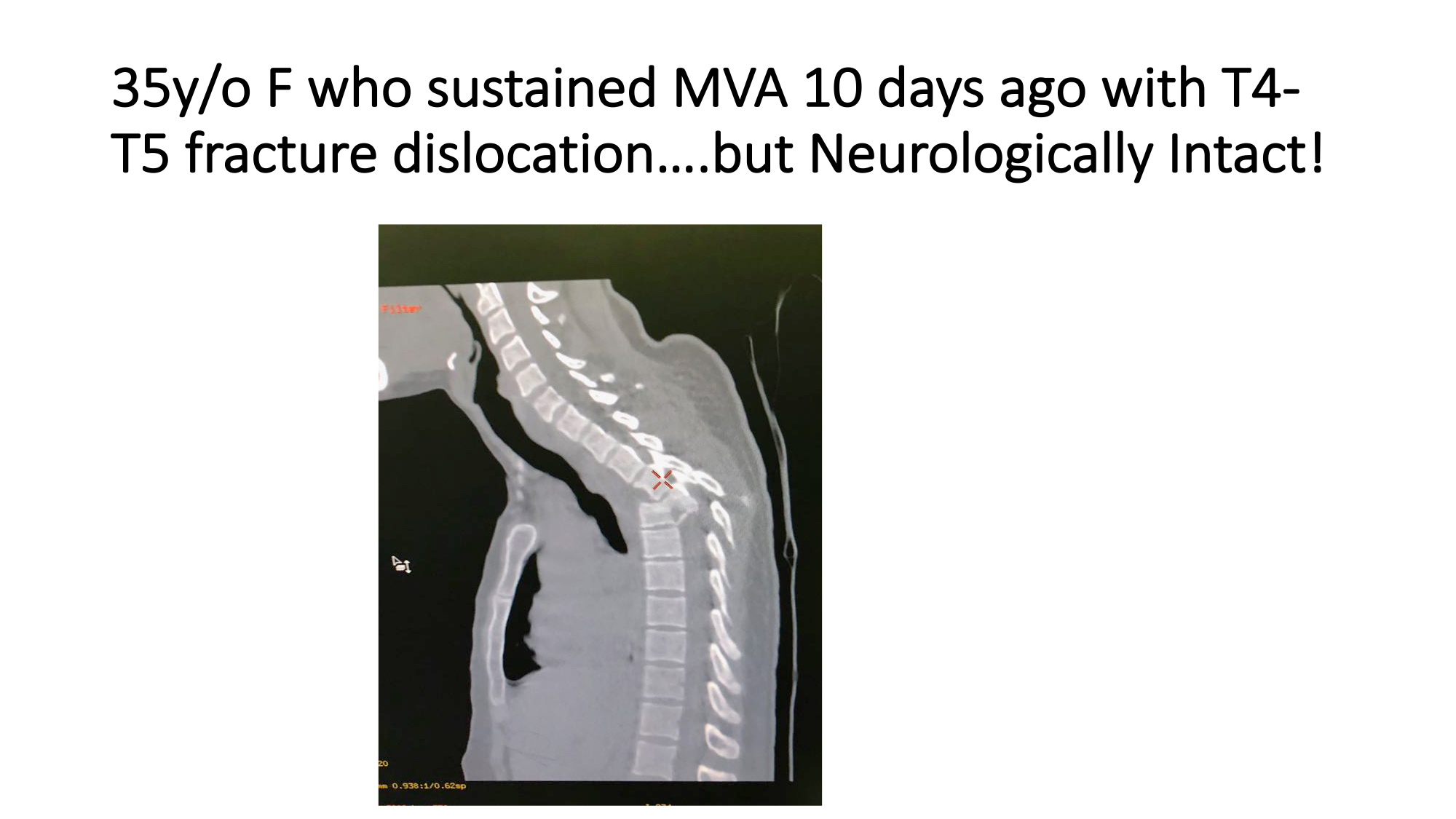
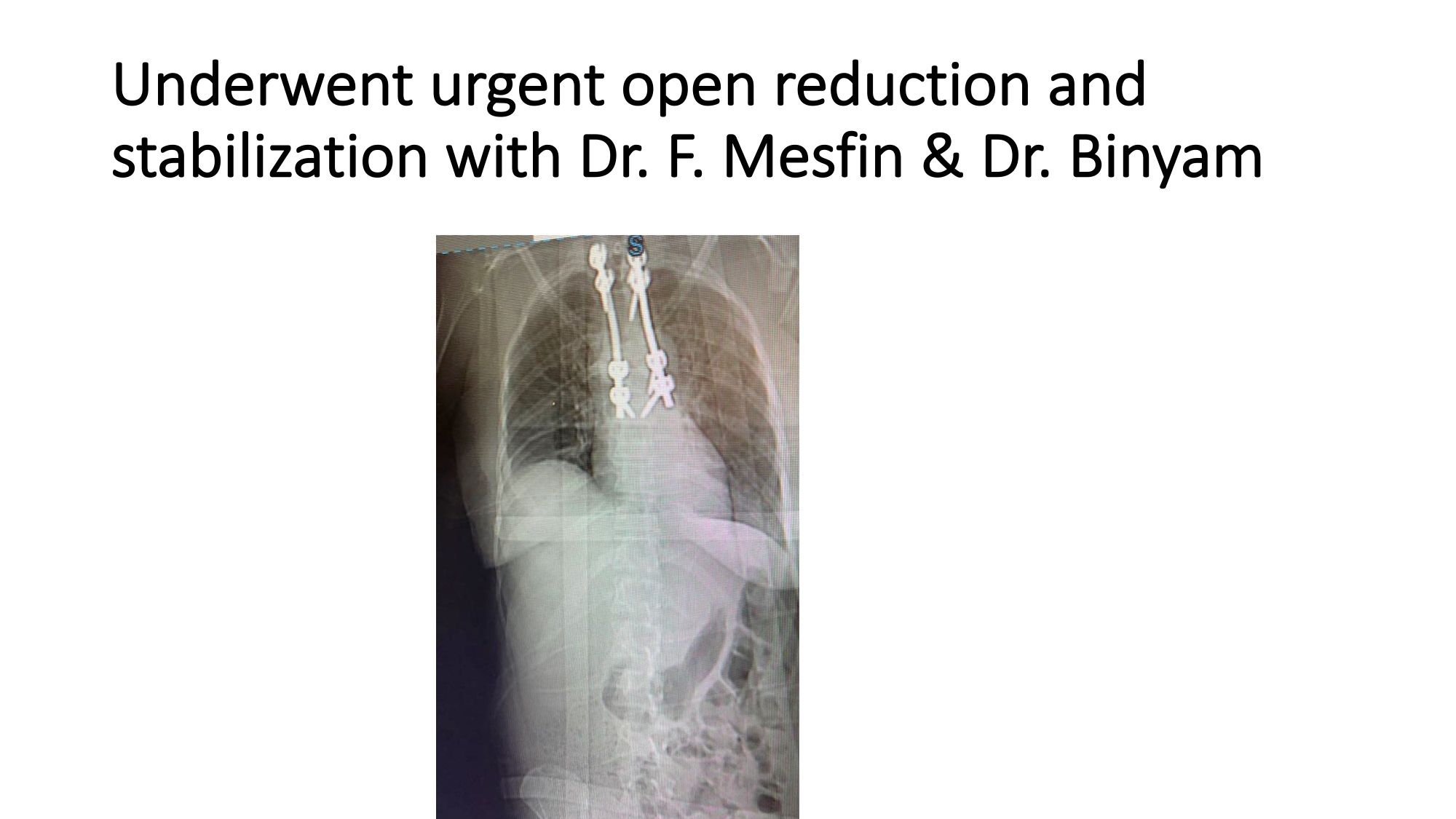
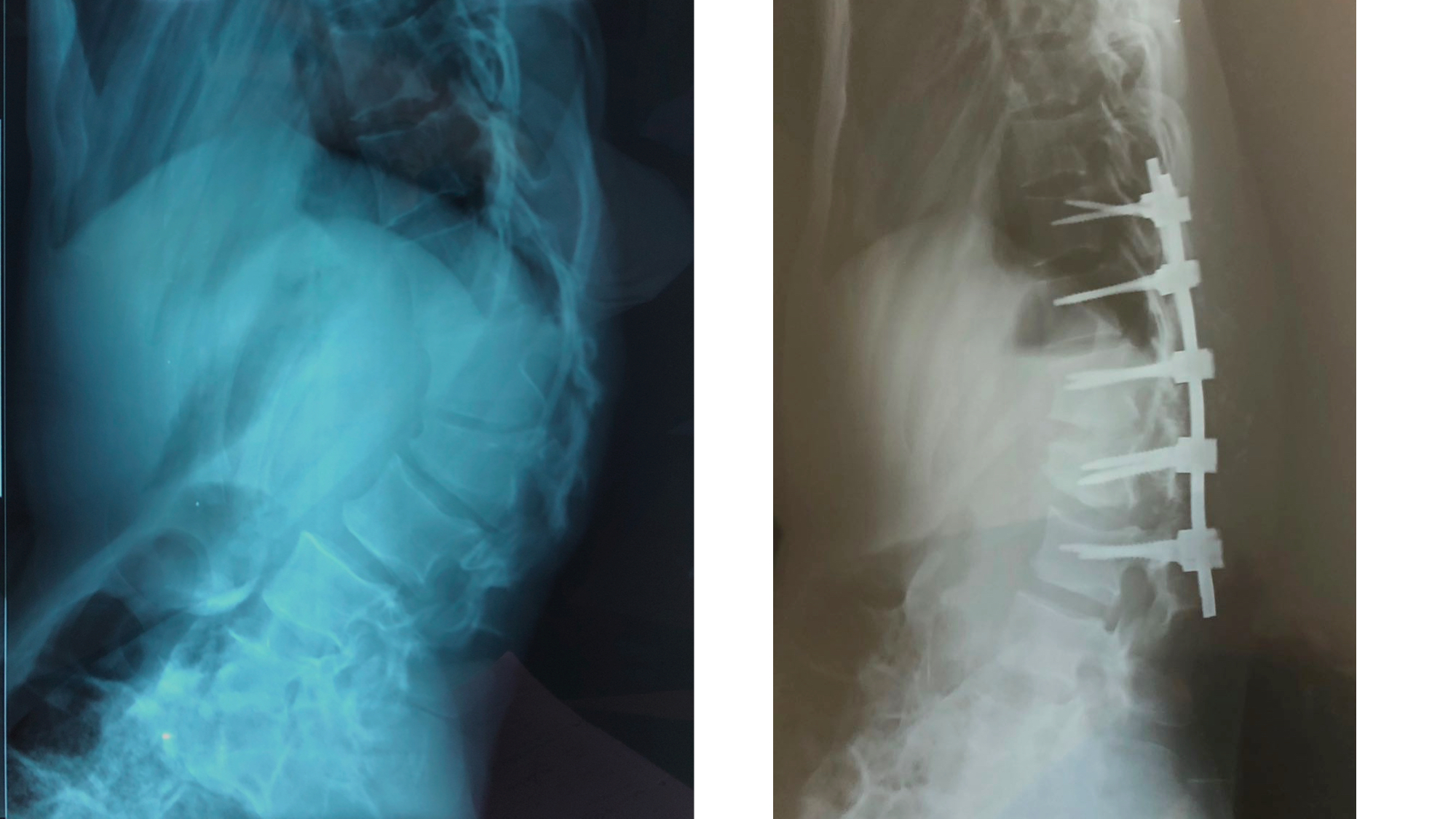
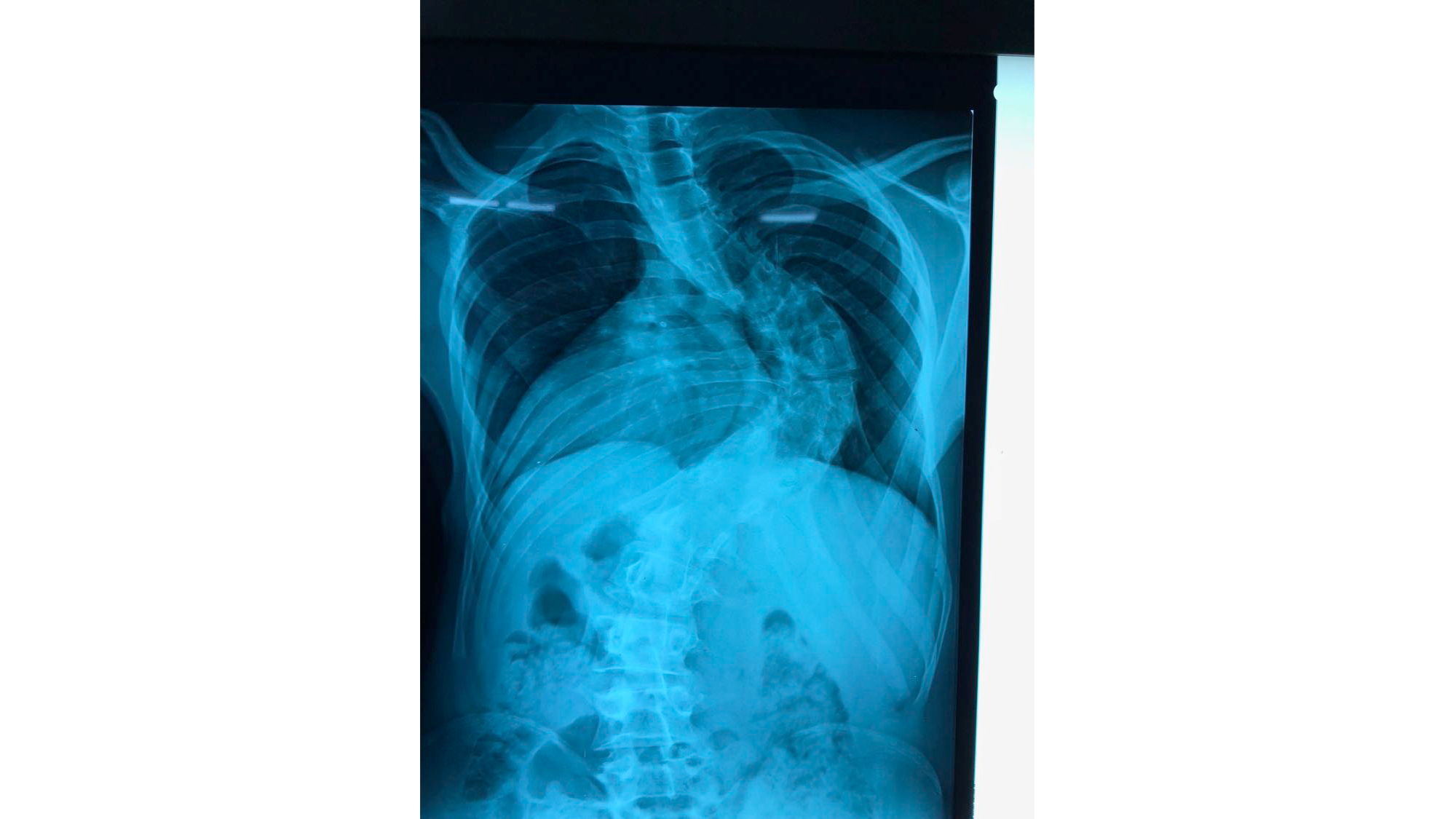
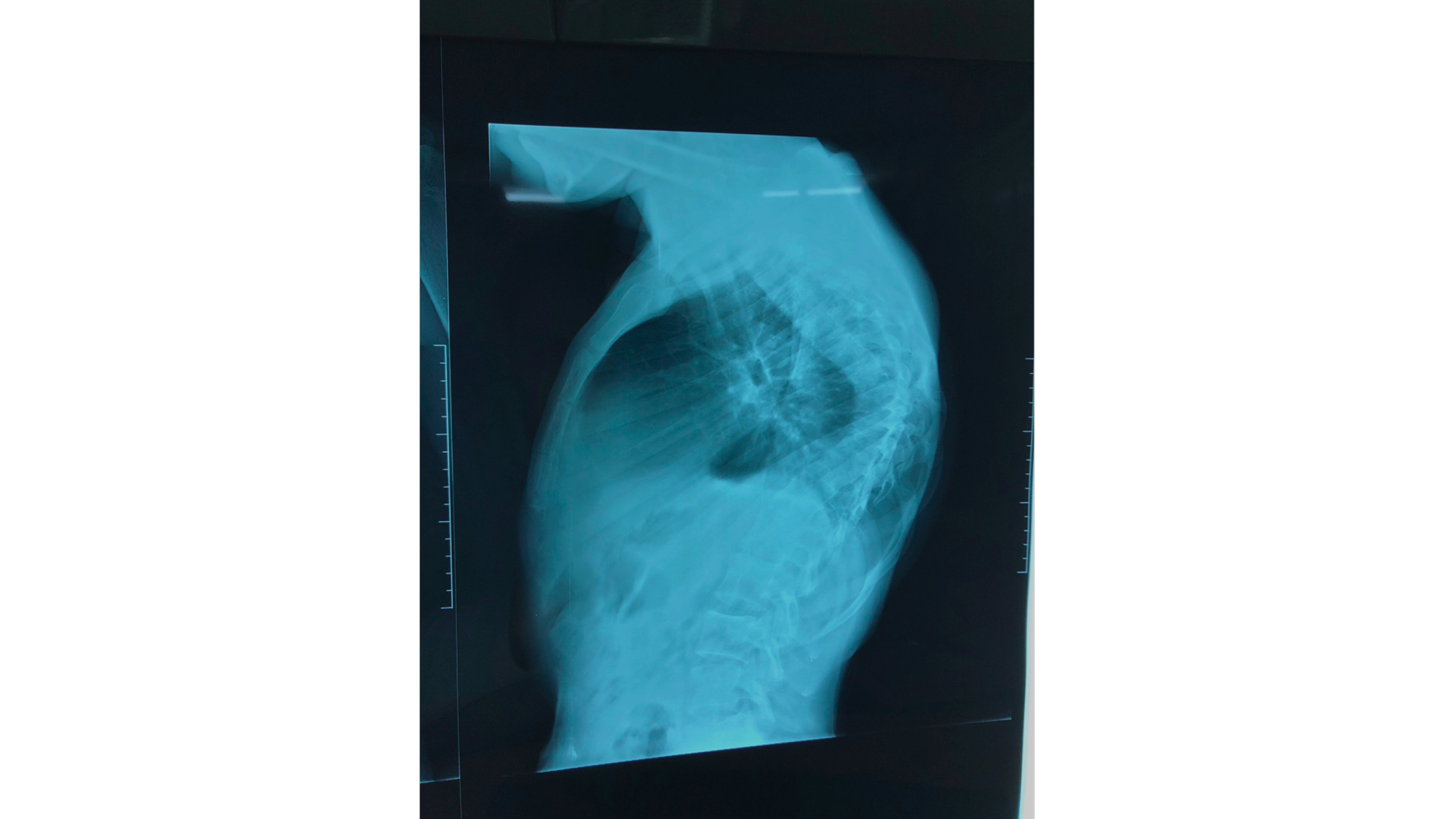
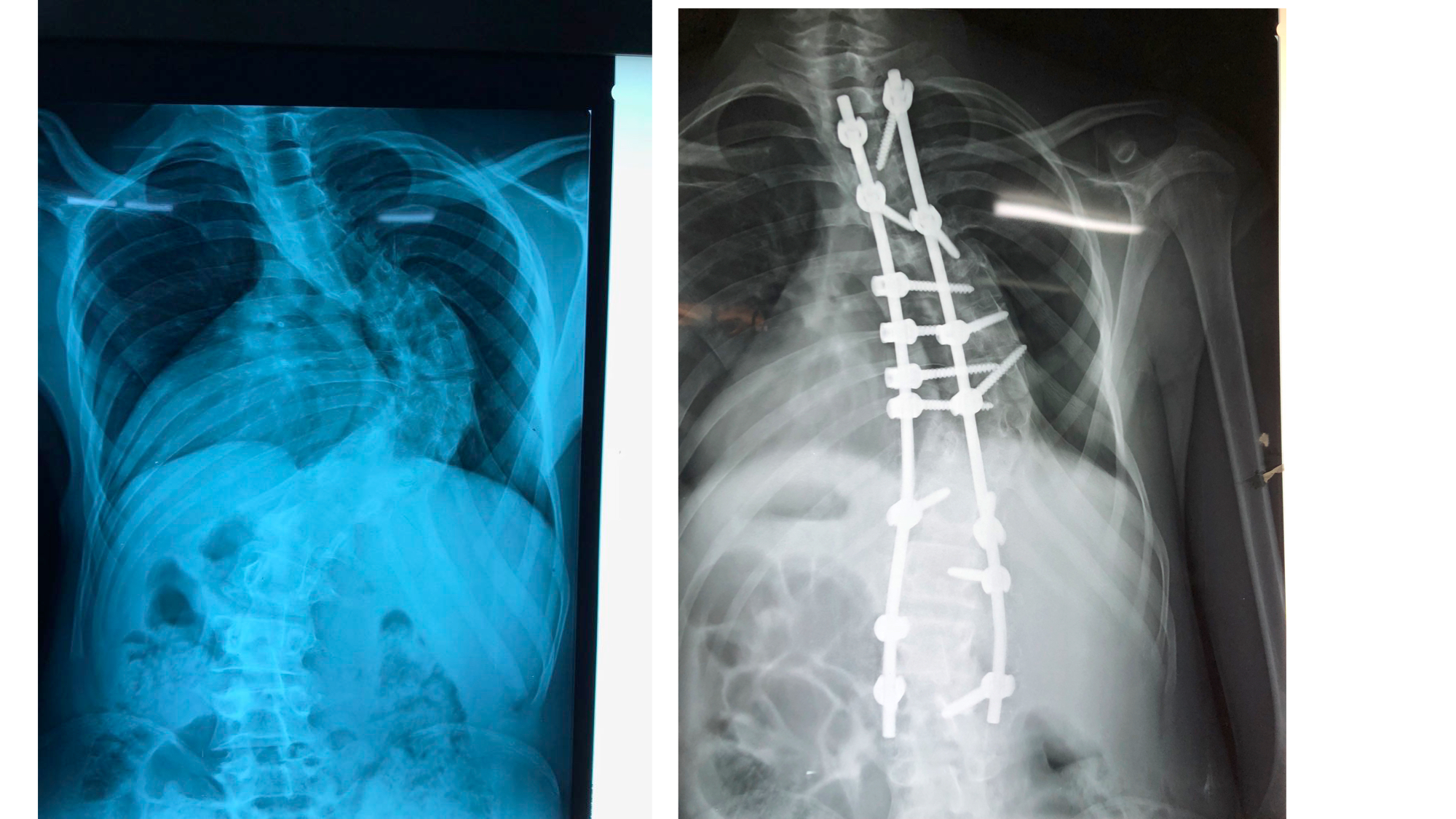
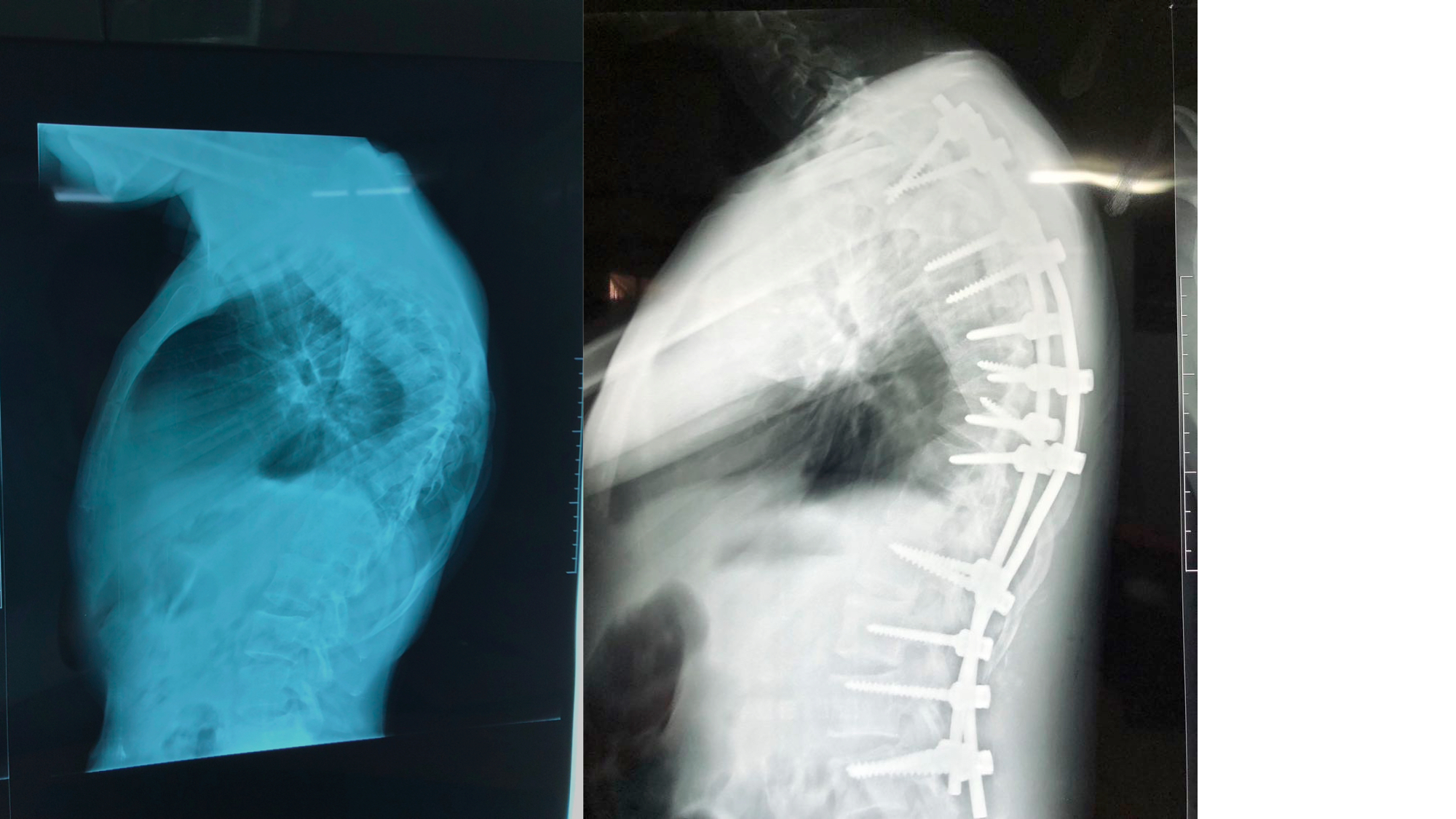
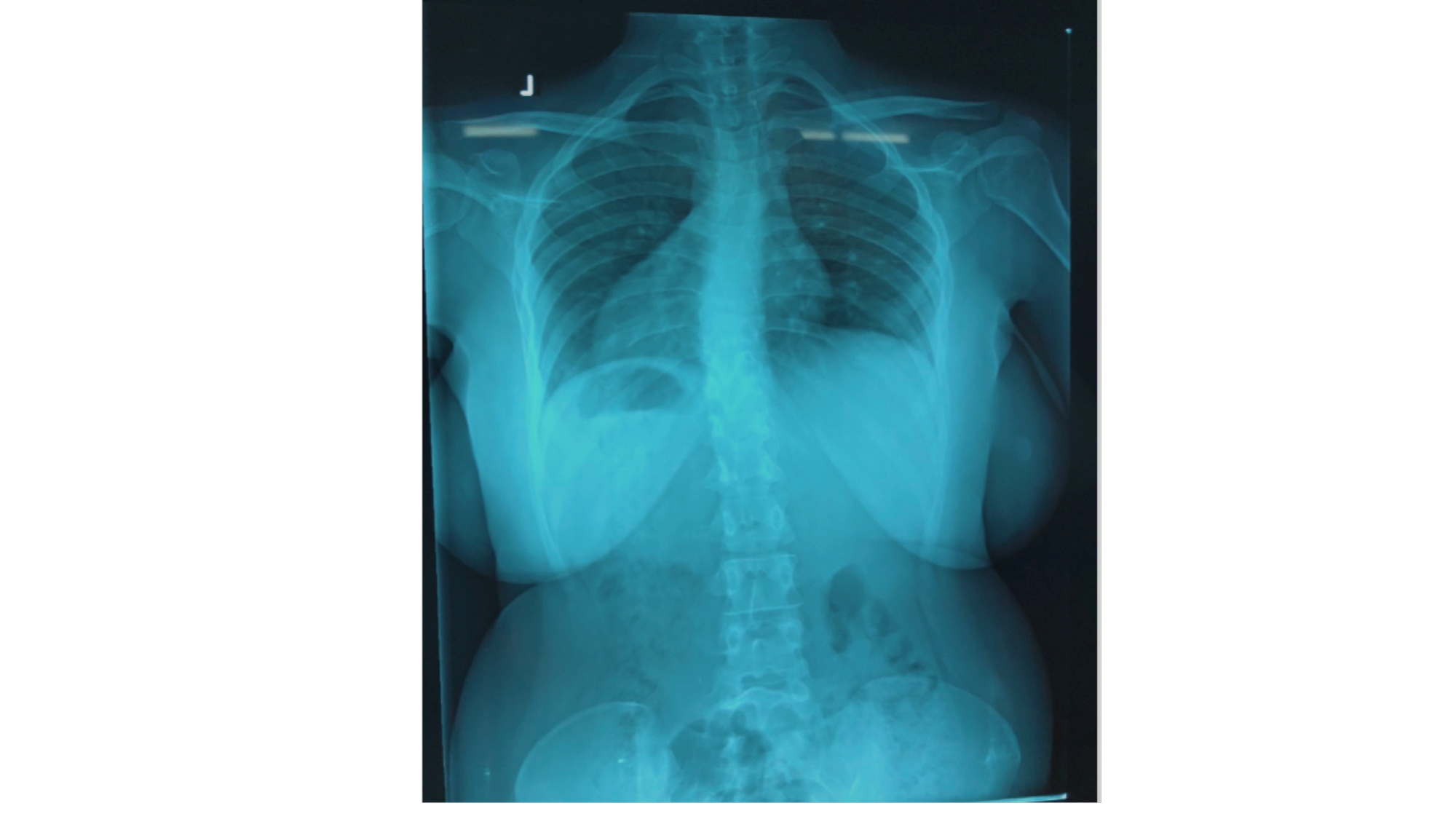
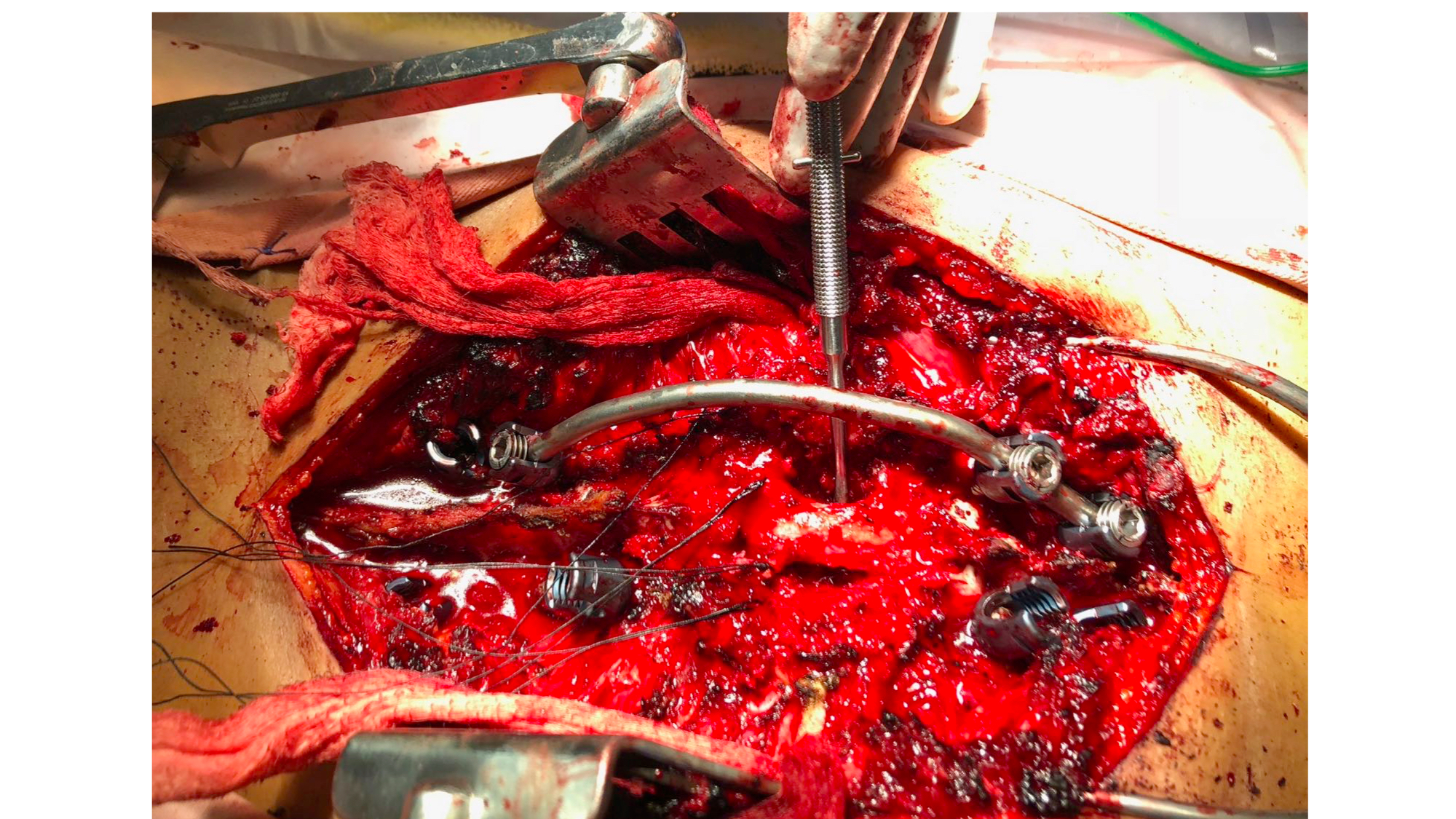
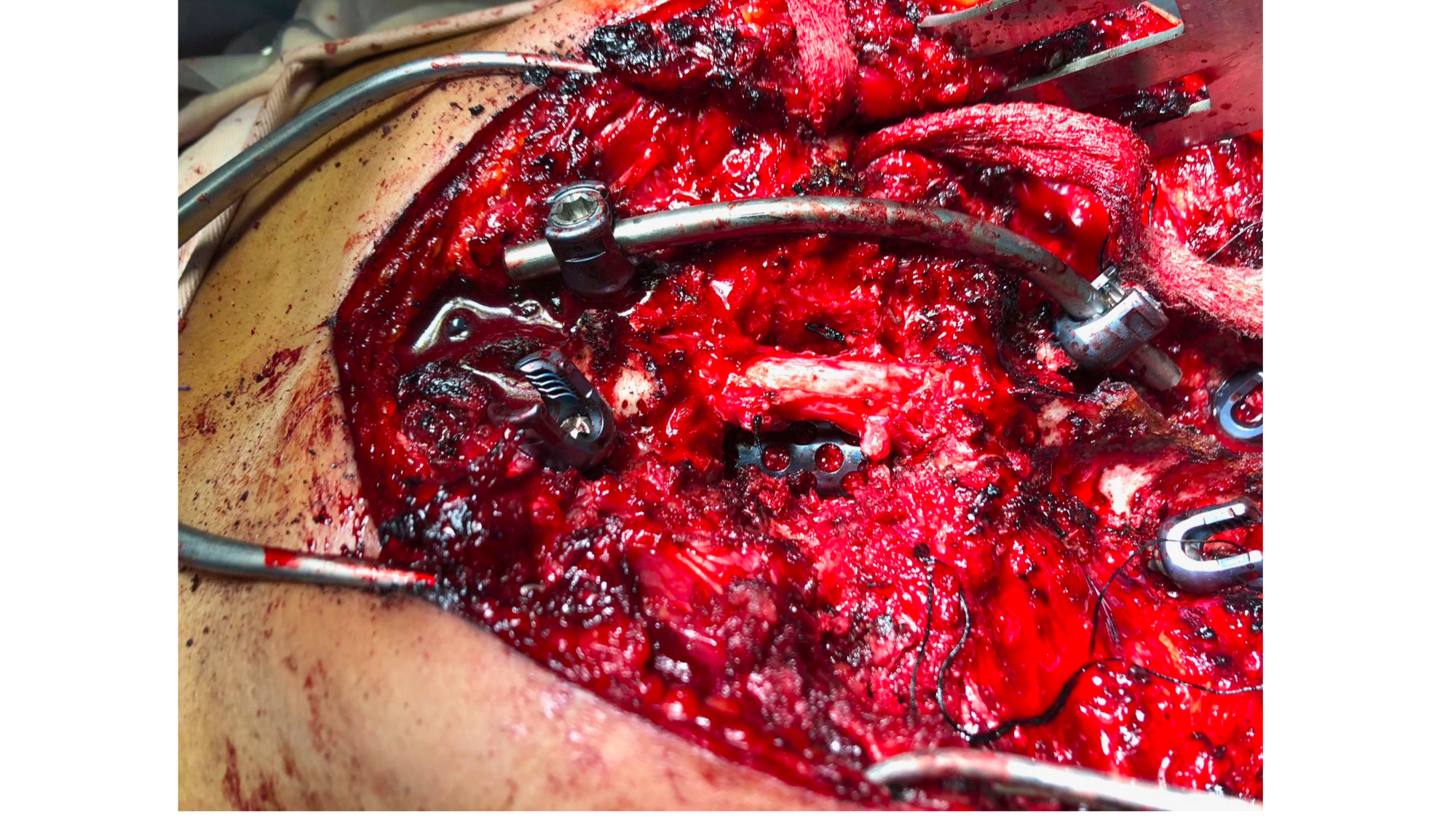
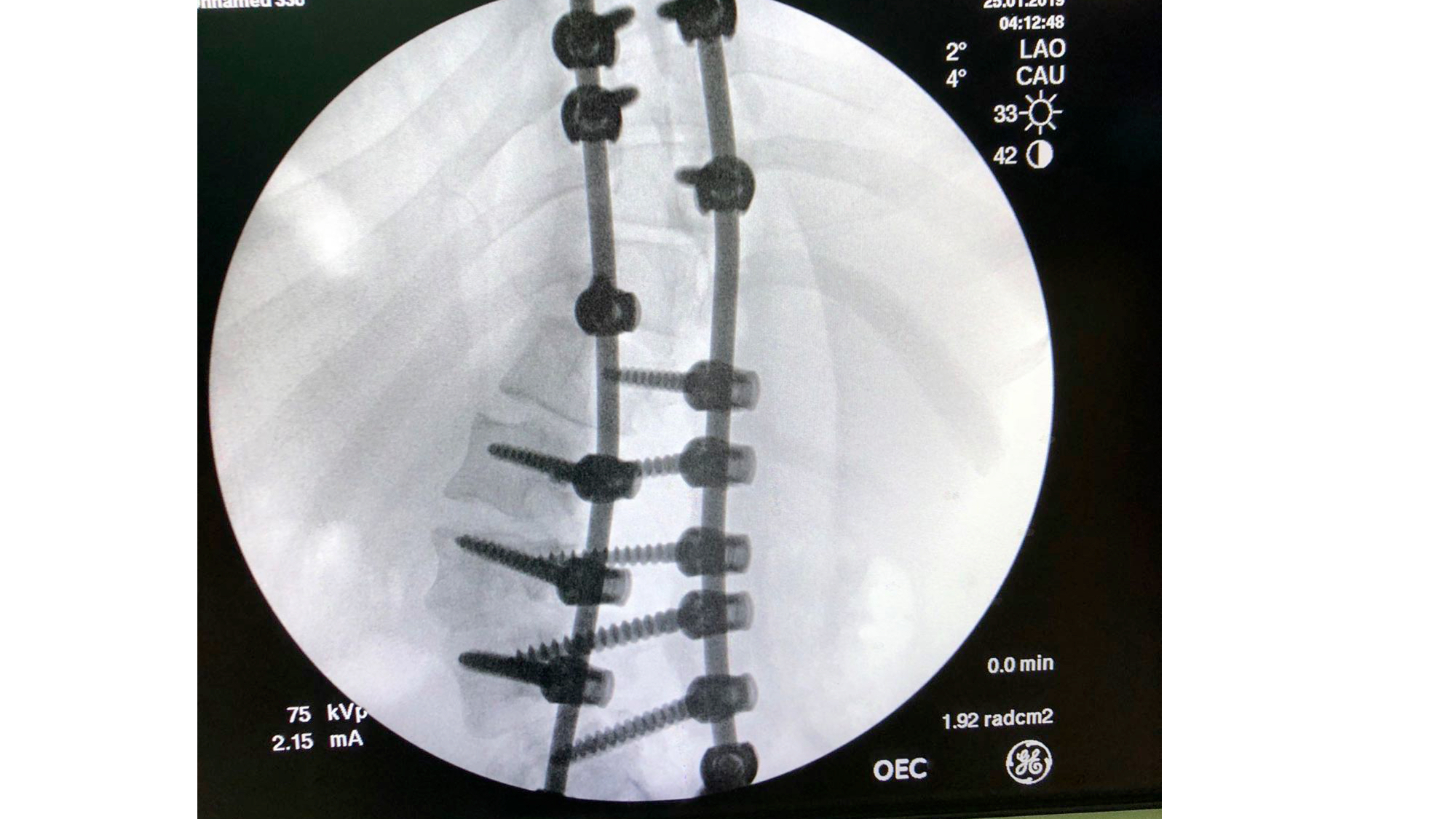
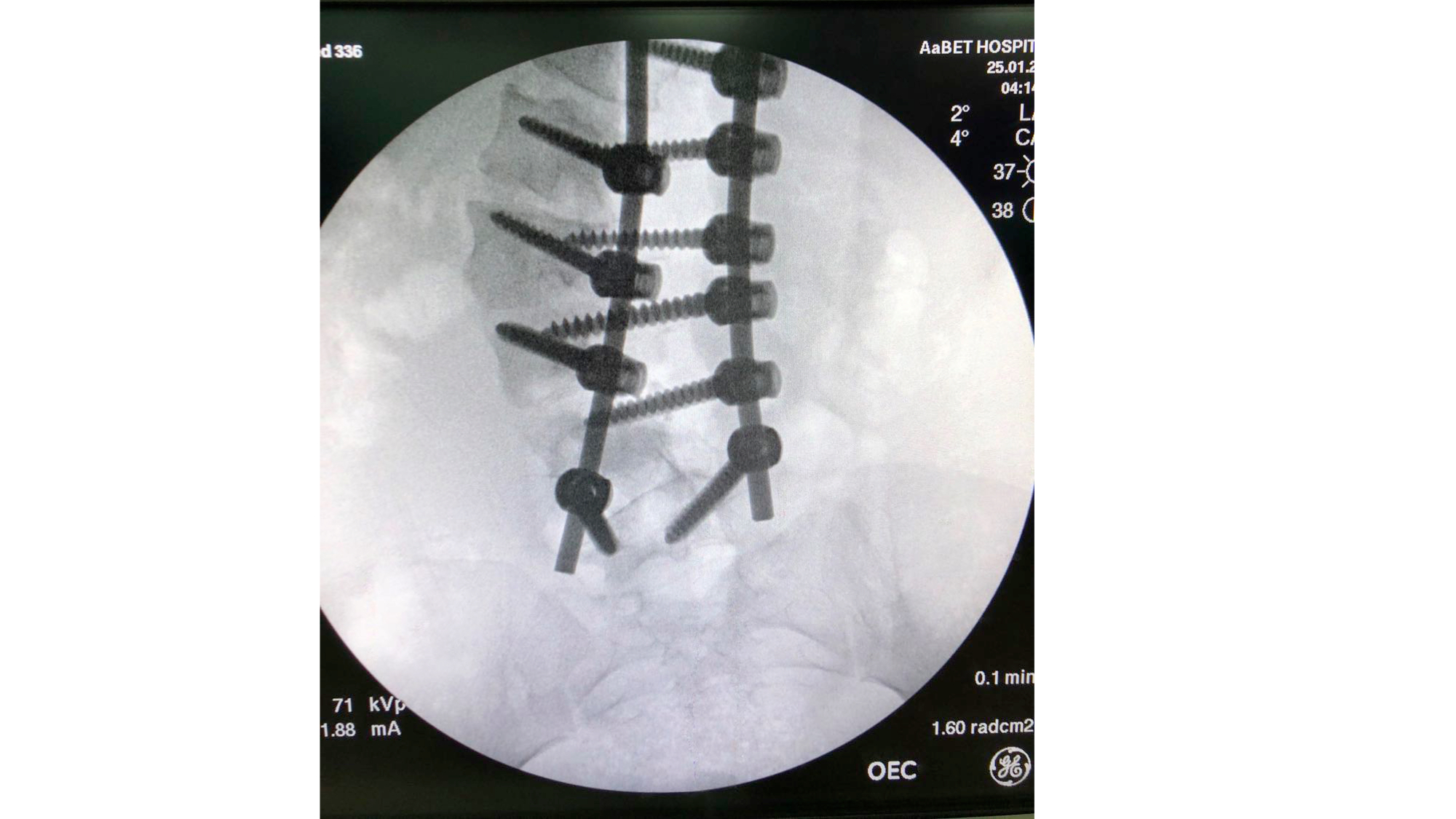
I was also able to meet the first two spine surgery fellows at AaBET. They are both neurosurgeons. The plan after next year is to alternate orthopedic with neurosurgery spine fellows. In addition to their teaching at AaBET, they are mentored by Dr Fasil Mesfin of Univeristy of Missouri, with whom they have weekly cases conferences. They were excited to show me two massive spine tumors they just operated on, one a giant, dumbbell shaped neurofibroma of the lower thoracic spine with bone involvement and preoperative paraparesis; the other a huge aneurysmal bone cyst of posterior lumbar element. Both needed pedicle screw instrumentation and big exposures. I am not a spine surgeon but the operative photos and postop xrays were very impressive.
Dr. Mamo and I then drove over to Black Lion hospital and went to a popular lunch spot across the street. Dr Ermias came to join us, the first MSK oncology trained surgeon in Ethiopia. He did his fellowship in Glasgow and has been in practice at Tikur Anbessa for a little under 2 years. A second oncology surgeon, Dr Samson, was trained in Milwaukee and is working in Sodo hospital in the south, doing oncology and reconstruction. He will be joining Dr Mamo and a few other surgeons later this year in their newly hospital and clinic “Dream Orthopedics” (more on this below). A little later Dr Getahun, my host at Ayder hospital, joined us. He is currently in the midst of a 1 year trauma fellowship with Dr Geletaw, who also joined us later.

We had lovely time chatting, while lunch and drinking coffee. Both Drs Geletaw and Mamo have successful part time private practices. Dr Mamo is working with my old UCSF classmate Tewodros Gedebou at Marsha clinic. The business model is that space and adminstrative support are provided freely but surgical revenue is split between the clinic and the surgeon.
It was great to finally meet Dr Ermias.He has a weekly multidisciplinary tumor board on Zoom. He collaborates with with the pediatric oncology service at Black Lion but due to scheduling conflicts they have not been able to attend each others’ tumor boards. He told me that copies of my textbook that I donated in 2019 are still circulating among the residents and remain appreciated.
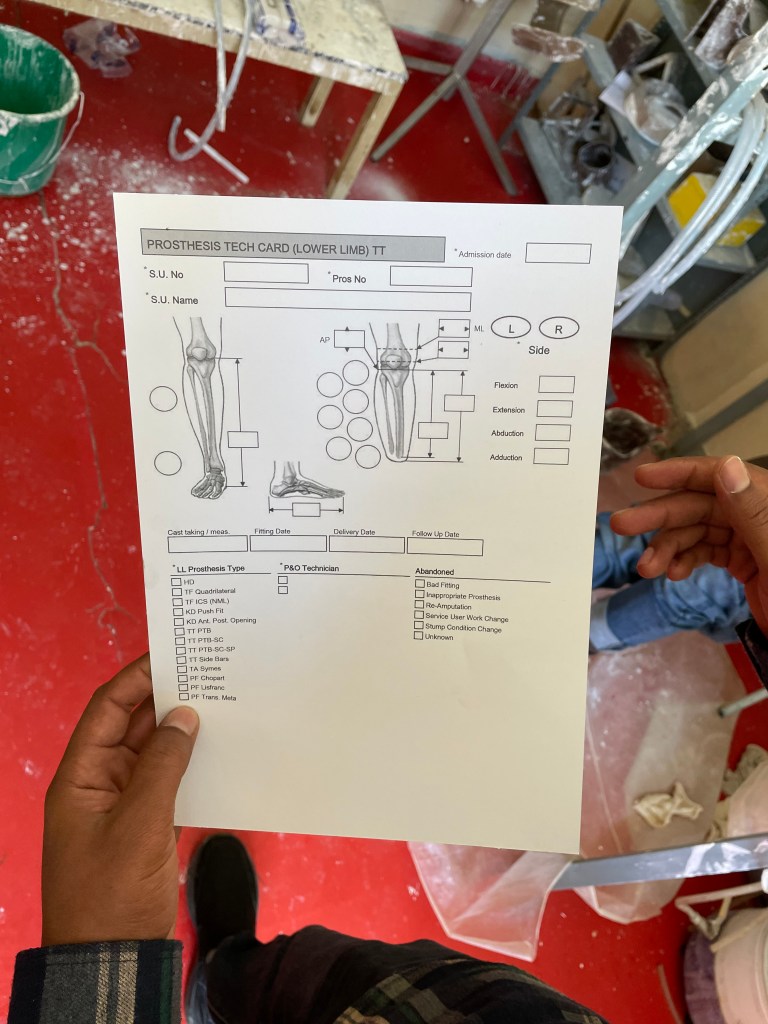
The challenges he is facing are the ones that would be expected. Modular prostheses are too expensive and thus most bone sarcoma surgeries remain amputations. MSK pathology expertise is not fully developed. Most patients with primary tumors arrive late and with advanced disease. For soft tissue sarcomas, tumors are often very large and plastic surgery support is needed. This makes cases even longer and there is already not enough OR time to handle the patient volume, so treatment is often delayed. Especially during the war, when all orthopedic capacity was diverted to war wounded, these delays led to some patients becoming inoperable. Even when there is a chance of cure for primary bone sarcomas, some parents resist amputation. I
proposed the idea of providing support for him to come to the annual MSTS (US orthopedic oncology society) meeting. He was very excited about the opportunity. It will take a little fundraising on our part and letters of invitation for him to get a visa, but both of us agreed it would be very helpful for networking and his continuing professional development.


Afterwards, Dr Mamo took me to the still being constructed “Dream Orthopedics and Trauma Center.” Theirs is a big vision to provide 24/7 trauma care, including general surgery, cardiovascular and orthopedic surgeons. It is a new multi-story building, with 41 patient beds, private “VIP” rooms, 3 ORs, ICU, radiology, lab, CT scan and ambulance entrance. It was launched as a partnership by 5 surgeons backed by an Ethiopian medical entrepreneur who provided capital and access to loans, in return for equity. Mamo is the CEO and has spent the last 1 1/2 years immersed in the construction details, equipment acquisition and I’m sure a million other details. It is located near the old OAU headquarters, so in a central location. I am sure they will be very successful, and I am very happy for him.
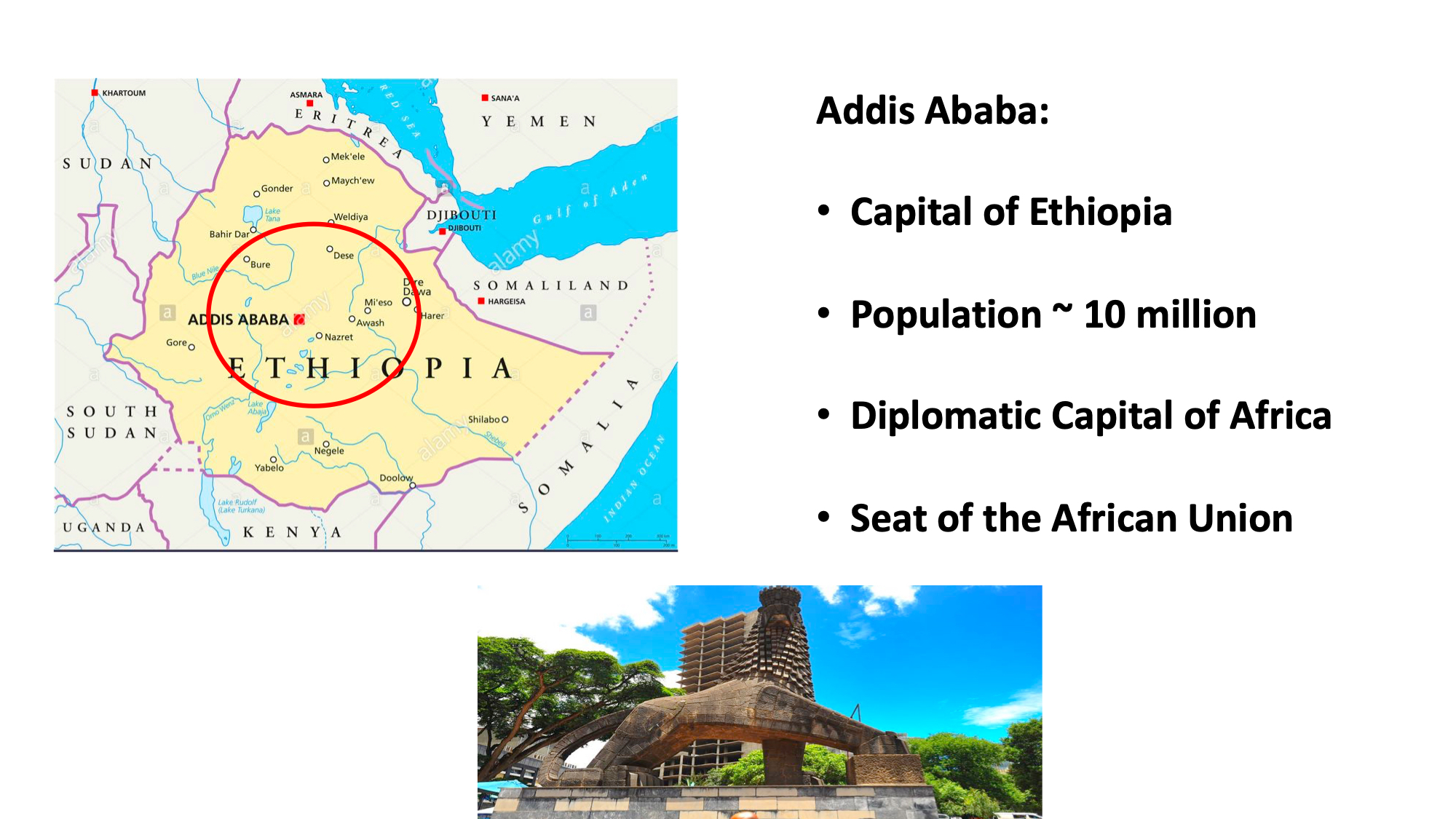
That was the end of my trip. The next morning I returned to Washington DC with a much clearer idea of the challenges in Tigray. I also saw first hand the incredible economic development in Addis, which will clearly soon be a health care destination for Africa. I also have many ideas of ways to make an impact, which will keep me busy for the next few years.